Cataract surgery provides many people with clearer vision in old age. Meanwhile, the operation belongs to the standard repertoire of many doctors. However, complications occur in about 5% of all operations performed.
About exactly these, we would like to speak here somewhat more in detail. In most cases, patients see more clearly after the operation and have no problems at all. In some cases, even glasses are no longer needed.
In some cases, areas of the eye are permanently altered by the surgery and a deterioration of vision may occur. Some deterioration is temporary and can be easily treated while others are permanent. It is important to filter out patients in advance who are at higher risk of suffering complications from cataract surgery.
These complications may be more likely due to anatomical conditions, or specific pre-existing conditions. Depending on the circumstances, the doctor can then adjust the surgery or equipment to best suit the patient and avoid problems during surgery.
INTRA-OPERATIVE COMPLICATIONS

Zonular dehiscence
IN 0.46% OF cases, instability of the lens occurs due to rupture or stretching of the zonucary fibers. In such a case, the surgeon may have to place additional iris hooks during the surgery to ensure the uniform fit of the new lens. However, other aids such as a ring could also be used.
This distributes the tension evenly. These rings sit at the equator of the lens in the capsule and support the lens by transferring the tension to the zonule. The stabilization of the newly inserted lens is particularly important, since a poorly fitting lens will also change the spectacle values required later.
Posterior Capsular Rupture
By far the most serious risk factor in cataract surgery is an occurrence that every cataract surgeon tries to avoid: Statistically, posterior capsular rupture occurs in 400 surgeries, in most of these cases associated with vitreous detachment.
The eyes with posterior capsular rupture and vitreous loss have a significantly increased risk of manifestation of amotio retinae. As a consequence, despite the replaced lens, there could be a deterioration in visual performance that cannot be subsequently restored.
Suprachoroidal Haemorrhage
Suprachoroidal hemorrhage is very rare in cataract surgery. Only 0.04% of patients experience this complication. They occur as a result of unexpected rupture of vessels in the suprachoroidal space.
Similarly, cataract surgery with larger incisions can have devastating consequences if intraocular pressure suddenly rises and ocular contents leak through the surgical wound.
Circumstances that make this complication more likely are the following:
- High intraocular pressure
- Advanced age
- Cardiovascular disease
- High blood pressure
POST-OPERATIVE COMPLICATIONS
Posterior capsular opacification
Months or years after cataract surgery, a secondary cataract (capsular fibrosis) may occur. This is not a new cataract. The cloudy lens of the eye has been completely removed during the operation. However, the lens capsule can become cloudy again.
The artificial lens was inserted into this capsule during the operation. A cloudy lens capsule is treated with a 5-minute laser procedure. The visual acuity rapidly increases again afterwards. The strength of the glasses does not usually change as a result of this laser intervention.
Raised Intraocular Pressure
As a result of cataract surgery, the intraocular pressure increases in individual cases, especially if glaucoma already existed before. However, the intraocular pressure may also decrease. Medicinal or surgical treatment may be necessary in case of changes in intraocular pressure.
Corneal Decompensation
Corneal endothelial cell loss after cataract surgery is reported in the literature to be 2% to 15% within the first postoperative year. The risk for corneal decompensation after cataract surgery depends on several factors.
- Core hardness
- Eye length
- Pseudoexfoliation syndrome (PEX)
- Diabetes mellitus
- Fuchs’ endothelial dystrophy
- Cornea guttata
As a result, an endothelial graft may be necessary because the natural function of the cells in the endothelium can no longer be maintained and the cornea becomes cloudy.
Endophthalmitis
Endophthalmitis is an infection inside the eye. It is a medical emergency. Eye surgery, eye injury, or infection in the bloodstream can cause this infection. Severe eye pain, redness of the eyes, and loss of vision can be the result.
Cystoid macular oedema
Cystoid macular edema is seen in the follow-up examination of the ocular fundus after 1-3% of uncomplicated cataract surgeries. It can be detected even more frequently with the help of contrast medium. In most cases there is a spontaneous improvement, only 10% of cystoid macular edema is still present after 2 years.
Retinal detachment
People who have had cataract surgery should be alert for the following signs, which may indicate retinal detachment:
- Seeing a dark “wall” or “curtain” in the eye
- seeing flashes in the eye
- seeing dark, moving dots or structures in the eye
If such symptoms occur, an immediate ophthalmologic examination must be performed. If a retinal detachment is diagnosed, surgery must be performed on the eye to preserve vision as much as possible.
Decentered lens
If the lens is not positioned exactly in the center, problems with visual performance may occur after cataract surgery. Especially if the cataract surgery was performed with multifocal intraocular lenses, which allow vision from distance to near. As a result, the patient would experience poor contrast in combination with glare at night.
Unplanned Refractive Results
The doctor makes every effort and uses high-tech equipment to calculate the optimal lens power. However, in practice, there are rare cases of unexpected results. In such a case, for example, a higher power of glasses may be needed on one eye, which may make the correction with glasses difficult and more likely to cause headaches. (Due to prismatic side effects).
Dry Eyes
A feeling of dryness can also occur after surgical procedures on the eye such as cataract surgery. Those affected have, for example, fluctuating visual performance due to uneven wetting of the cornea. The deterioration of the tear film is related to the damage of the nerves during the surgeries.
Light sensitivity
Light sensitivity after cataract surgery is very common. The increased sensitivity of the eye to light is due to the retina. In the course of the disease, the retina has become accustomed to the reduced incidence of light due to the clouding. So, conversely, it has to get used to more light coming in again. However, light sensitivity after cataract surgery is not permanent. For the first time, it makes sense to wear sunglasses. These bring relief and protect the sensitive eyes at the same time from dust and wind.
Example for a Bad Experience After Cataract Surgery
In many cases, it is poor communication between the doctor and the patient when the surgery does not turn out as expected. In the picture below you can see a topography of a cornea. This is usually done before surgery to see how the cornea is made and how the refractive power is distributed.
As you can see here, the living surfaces are positioned differently. This means that there are different lens powers on the eye. The customer to whom the topography belongs opted for a multifocal lens.
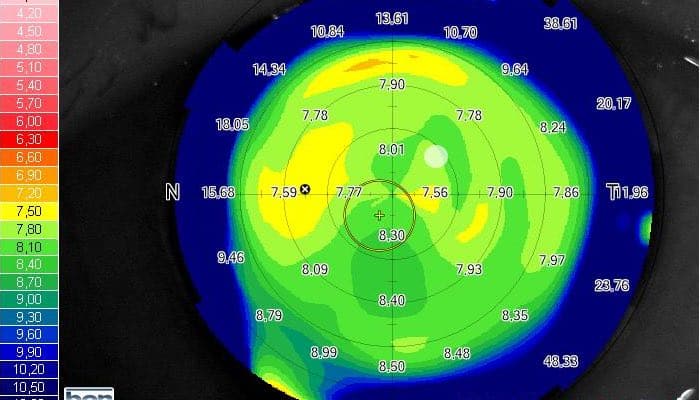
The problem now is that with such a topography it was already clear before the surgery that the visual performance will be somewhat impaired. So even before the cataract, she did not see everything crystal clear.
But that is what she expected. However, this is not possible due to the anatomy. In addition, there is a certain loss of contrast with a multifocal fitting. She would have liked to have more contrast.
The multifocal lens was also positioned somewhat off-center in this lady. The result is increased glare effects when driving at night, which she can no longer do. She feels restricted with the new lenses and must continue to wear glasses although she was told before the operation that this would no longer be necessary after the operation.
She now has to wear varifocals and feels completely misadvised. Rightly so. The bottom line is to always ask how far it is meant that you can see well without glasses.
Many doctors think that after a cataract operation you can expect to reach the optimal value. If you still need glasses after the operation, because you can only see sharply up to the room, this is a success.
Are you thereby completely free of visual aids? No. So define for yourself what exactly you want and ask the doctor how likely your wish will come true.
